Hundreds of thousands of animals are tortured and killed in the United States each year in cruel and unreliable animal tests.
Some of the cats, dogs, guinea pigs, hamsters, monkeys, rabbits, pigs, rats, mice, and sheep endure multiple experiments, being “recycled” from one study to the next. Others — including all animals infected during disease trials — are killed at the end of the experiments.
The United States used and killed more than 797,500 animals in research experiments in 2019 alone, according to the most recent data from the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (APHIS).
That massive number does not include rats and mice, who are not protected under the Animal Welfare Act, a federal law that establishes only minimal protections for animals used in labs who often endure painful procedures — including being burned, shocked, poisoned, mutilated, or brain damaged — without anesthesia.
The cruel animal testing is required for all new medical treatments by the Food and Drug Administration (FDA), via provisions established in 1938 that necessitate tests on at least two species: one rodent species, and one non-rodent species.
Those provisions remain in place despite decades of evidence highlighting key genetic differences between humans and other species: the reason that more than 90 percent of all drugs approved in animal tests fail once they hit human clinical trials, and why only 6 percent of vaccines make it to human markets.
While some scientific organizations, including those that rely on animal testing for funding, have used COVID-19 to promote animal testing as a “needed” approach, the scale and severity of the pandemic — and the urgent need for a quickly-developed vaccine — has highlighted the need to shift to safer, faster, and more reliable alternative methods for a growing number of scientists.
A study published in May 2020 in the Archives of Toxicology noted that the pandemic “clearly shows the shortcomings of an approach that invests 95 percent of resources into a single technology (animal experimentation) in the face of challenges that require alternative approaches.”
At the same time, in an unprecedented move, the FDA authorized Phase 1 human clinical trials to proceed at the same time as the required animal testing. That green light slashed the amount of time needed before the vaccines became available to the public.
Animal testing currently remains “the only way” to get drugs and life-saving medical treatments approved for human use, but scientists who spoke with Lady Freethinker and peer-reviewed studies published in renowned medical journals said it doesn’t have to be that way for the future.
Here we highlight three key takeaway lessons from the COVID-19 pandemic: animal tests inherently are cruel, costly, and unsafe. Humanity could be better served by shifting to safer, more humane, and more cost-effective human biology-based methods. We also have some action steps for animals that you can take after reading.
1. Animal Testing Is Cruel and Often Fatal for the Animals Involved
Thousands — if not millions — of mice, rats, hamsters, ducks, cats, guinea pigs, ferrets, and monkeys have died worldwide in the global race to find working COVID-19 vaccines, according to a report from Cruelty Free Europe.
While specifics of the tests differed, generally animal subjects were injected with vaccines and then “challenged” — or infected with high doses of the COVID-19 virus — by being forced to inhale the virus or having the virus introduced directly to their lungs via tubes inserted down their tracheas. All animals infected with COVID-19 were killed at the end of the tests — as is a common practice with infectious disease trials.
Animal Testing and the Pfizer Vaccine
The Pfizer vaccine involved tests on mice and male rhesus macaques, aged 2 to 4. In the mice studies, female mice were injected with a vaccine in their leg muscles and then exposed to high levels of the virus. Scientists drew blood from behind their eyes during the study, then killed the mice to examine their organs. The study does not note how the mice were killed, although carbon-dioxide gassing and neck-breaking are commonly used and accepted methods.
In the monkey studies, scientists injected the vaccine into the leg muscles of the test animals, then infected them with the virus 55 days later by forcing the animals to inhale the virus or inserting it into their lungs via a tracheal tube. The animals then endured having their blood drawn and lung samples taken multiple times, along with multiple nose and throat swabs, before the infected monkeys were killed, seven to eight days after being infected. Monkeys who had not been infected were infected to continue the research, according to the published study.
Dr. Avi Bitterman, in a panel discussion of vegan doctors about the vaccines, reported that a total of 106 animals — 64 mice and 42 rhesus macaques — were used and killed in Pfizer vaccine test trials. He said going through clinical data for Moderna’s vaccine was trickier but that the number of animal deaths was likely similar.
Animal Testing and the Moderna Vaccine
The Moderna vaccine was tested on mice, hamsters, and rhesus macaques. Moderna’s mice received vaccine injections into their leg muscles. Five to 13 weeks later, they were infected with high doses of a “mouse-adapted” COVID-19 virus, then killed so scientists could examine their organs. Syrian hamsters underwent a similar set up, first being injected with vaccine and then three weeks later being forced to inhale high doses of the virus. Scientists killed hamsters two to four days after infecting them, with the study mentioning only that the animals were “killed serially.” The unvaccinated, ‘control’ hamsters were observed for an additional 14 days — during which they lost an average body weight of up to 12 percent — before scientists killed them at the study’s end.
Moderna’s test monkeys — both males and females, ages 3 to 6 years old — received two injections of either a low or high dose of vaccine into their leg muscles, then four weeks later were infected with high doses of COVID by being forced to inhale the virus or having the virus inserted via tracheal tubes into their lungs. They endured having their blood taken at least four times, as well as multiple nose swabs and lung samples, before being killed seven to eight days after being infected.
According to published clinical data that LFT tracked down, the Moderna vaccine tests killed at least 24 rhesus monkeys, 45 hamsters, and an unidentified number of mice.
Animal Testing and the Janssen Vaccine
The Janssen (Johnson & Johnson) vaccine involved tests on mice, rabbits, Syrian golden hamsters, and monkeys. Scientists gave hamsters a single dose of vaccine, then four weeks later infected the animals with low or high doses of COVID-19 before killing them starting two days after infection to examine their organs. Hamsters who received a low level of the virus lost about 15 percent of their body weight by the sixth day of the study, while hamsters who were infected with high levels of the virus lost up to 20 percent of their body weight and became so sick from weight loss and breathing problems that they met scientific criteria to be “humanely” killed.
Janssen’s tests on monkeys involved single doses of vaccines, followed by infections six weeks later. The animals endured similar procedures as those in the Pfizer and Moderna trials before being killed and examined.
According to published clinical data that LFT tracked down, the Janssen vaccine used or killed at least 52 monkeys, at least 60 Syrian golden hamsters, and an unspecified number of rabbits and mice.
Other Animal Victims of COVID-19 Experiments
- The Oxford/Astra Zeneca (U.K) vaccine studies involved at least nine rhesus macaques: six of whom were vaccinated and exposed to the virus, and three of whom were exposed to the virus without vaccination. All nine monkeys became infected and showed symptoms including rapid breathing.
- The Sinovac Biotech (China) vaccine studies injected at least 10 rhesus macaques with two different doses of vaccine before exposing the monkeys, plus at least five unvaccinated monkeys, to the virus. Unvaccinated monkeys developed severe pneumonia before being killed.
Other animal victims of COVID-19 included thousands of horseshoe crabs caught and bled to test vaccines for possible toxins and animals culled in unrelated lab experiments when COVID-19 shut down universities.
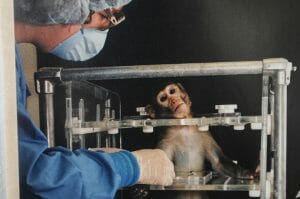
A representative image of monkeys used in experiments (Photo Credit: We Animals)
2. Animal Testing Is Unreliable and Costly for Both Animals and People
The COVID-19 pandemic highlighted genetic differences between humans and the animals used in testing.
Mice and monkeys, used to test all three of the U.S. vaccines originally approved for emergency use, were not naturally susceptible to COVID-19, nor did they develop as severe of symptoms as humans. Some researchers chose to first create “co-morbidities” in some of the animals — like hypertension or diabetes — to get the animals’ responses to more closely resemble human symptoms, according to Science. Moderna’s scientists also infected their mice with a “mouse-adapted” strain of COVID-19.
In an alarming discovery that could spell future disaster for humanity, researchers at the University of Bristol reported that the COVID-19 virus can mutate in monkey tissue — meaning that testing involving COVID-19 on animals could actually create new variants.
Scientists already have known for decades that significant genetic differences exist between humans and other animals. Even the National Institutes of Health (NIH), which operates seven U.S-based research facilities involving monkeys, noted that “animal models often fail to provide good ways to mimic disease or predict how drugs will work in humans, resulting in much wasted time and money while patients wait for therapies.”
The unreliability of animal testing, and the corresponding lengthy approval process, adds up to new drugs taking an average of 10 to 12 years to go from concept to drug store shelves, with an average development cost of $2 billion, according to estimates from the Center for Alternatives to Animal Testing (CAAT) at Johns Hopkins University.
A single macaque monkey for research can cost more than $10,000, and the United States blew through more than 68,200 macaque monkeys for research in 2019 alone, according to the most recently available data from the U.S. Department of Agriculture’s Animal Plant and Health Inspection Service (APHIS).
The deadly demand for monkeys in the global race for COVID-19 vaccines exacerbated an already existing “shortage” of monkeys that has led research-heavy companies, including the National Institutes of Health (NIH), to say they can no longer meet the demand for medical and psychological experiments.
The U.S. Government’s response has been to pitch a 27 percent increase to NIH’s 2022 budget — to the tune of $30 million, taxpayer-supported dollars — to aid the agency with purchasing more monkeys for experiments and otherwise funding their monkey-based operations.
A study published in the Cambridge Quarterly of Healthcare Ethics by Aysha Akhtar, a double Board-certified neurologist and a former medical officer for the FDA, outlines the flaws inherent in animal testing as far back as 2015.
Akhtar co-founded the Center for Contemporary Sciences (CCS) to develop faster, more cost-effective, and more humane alternatives to animal testing.
“Medical science should be focused on understanding human biology, not on the biology of a rat, a cat, a dog, or a monkey,” CCS wrote in a blog post. “It seems so logical, doesn’t it? But to transform the biomedical research enterprise, we need to unlock ourselves from old ways of thinking.”
“For the sake of human health, our tax-dollars should be directed into the best science,” Dr. Akhtar continued, in a post published by TruthOut. “Whichever way you look at it, future biomedical research, including vaccine development for pandemics like COVID-19, will be based on human biology and human-specific testing methods. These methods are quicker, cheaper, more humane, and — most importantly — relevant.”
Akhtar told Lady Freethinker that proves especially true with the case of vaccines.
“The whole point of a vaccine is to boost our immune system, to get it primed and ready should we encounter an infection,” she said. “Immune systems are very species specific. Researchers couldn’t find a species that got COVID-19, or showed symptoms the way that humans do, and that delayed the process.”
The fact that researchers needed to create comorbidities — or underlying conditions that plague unhealthy humans, such as obesity or diabetes — in test animals added in concerning variables.
“Comorbidities were artificially introduced to these animals,” Akhtar said. “So you are dealing with artificial diseases. These are not the diseases that humans get. People should absolutely be concerned with the genetic differences between species.”
The quickest vaccine previously created was for mumps, which took four years. On average, vaccines take 14 to 17 years, Akhtar said.
“What happened with the COVID vaccine was unprecedented,” she said. “It happened because combatting COVID-19 became a global priority. But that also raised the question of why are we still doing animal testing, when the gold standard for humans should be human biology?”

A representative image of a hamster, an animal increasingly used in animal tests. (Olga Skred / Alamy Stock Photo)
3. Animal Testing Is Only Necessary Because of An Outdated Law That Should Be Changed
The current animal testing requirements in the United States harken back to a law passed in 1938, which requires animal tests before medical treatments can pass to human clinical trials.
In the almost century since, scientists worldwide have created innovative, human-biology based methods that could readily serve as substitutes for unreliable, cruel, and costly animal testing: from organ-on-a-chip, organoids, and 3D-cultured artificial human lymph nodes, cell cultures, and tissues to spheroid models, in silico approaches, bioreactor cultures, and microphysiological systems.
But because the law remains unchanged, scientists have no choice but to test on animals — even if that outdated requirement means finding safe treatments will take longer, cost more, and involve preventable harm to human volunteers who test possibly unsafe drugs during Phase 1 clinical trials.
“The argument that we need animal testing is so wrong,” Akhtar told LFT. “Ninety percent of drugs fail, because they end up being unsafe or ineffective for humans. That shows that animal testing is unsafe and unreliable and that we need a new system.”
While some scientists have said the simultaneous animal and human clinical tests for COVID-19 vaccines might prove “unwise” in retrospect, other scientists have said the simultaneous tests allowed for the creation of safe and effective vaccines. Moderna’s chief medical officer told Stat News, “I don’t think proving this in an animal model is on the critical path to getting this to a clinical trial.”
Akhtar said she sees both short- and long-term likelihoods for the future of animal testing, based on repercussions from the pandemic. She said a short-term impact likely will be a continued, unwarranted demand for animals but added that continued reliance also will serve to underscore the tests’ unreliability.
“These efforts are underway even though using animals as human ‘models’ for decades has not led to any effective treatment for most diseases,” CCS wrote on their website. “It doesn’t make sense to continue the same old system when we know the system is broke.”
Akhtar is optimistic that the long-term takeaways from COVID-19 will be an increased call for superior, human-biology-based methods.
“Even if experimenters succeed in increasing funding toward animal use, I predict the effect will be limited,” she said. “The pandemic has highlighted the need for testing methods that are reliable, effective, safe, and fast.”
While scientists who promote animal testing are pointing to likely future pandemics as an alleged need to “stockpile” research animals, Akhtar said that same likelihood of new and serious diseases means humans need to adapt to innovative methods to survive.
“Ultimately we will only be able to stay ahead of viral mutations by focusing on human biological responses to the virus and to potential vaccines and drugs,” she said. “As a result, there has been a sharp focus on how human-specific testing methods can accelerate our understanding of viruses and pave the way for treatments.”
The FDA already has approved using alternative methods for some COVID-19 related tests, including chips with human lung cells for tests by Emulate Inc., lung organoid studies in Boston and San Diego that study effects of existing drugs on the virus, human-biology-based antibody tests by research group YUMAB, and organ-on-a-chip studies by Toronto researchers. The Oak Ridge National Lab in Tennessee also is using Summit, a supercomputer, to identify existing drugs that might be able to counter COVID.
Popular opinion also has shifted increasingly against animal testing, with less than half of Americans polled by PEW in 2018 saying they supported animal testing.
Akhtar said there was a slight dip in that number when the pandemic hit — a change she attributed to animal researchers “exploiting people’s fears.”
“Our media has done a poor job of allowing a narrative of the ‘need’ for animal testing to continue, despite the massive amount of scientific evidence,” she said. “There will be a day when everyone will look back and say, ‘We used to search for cures for human diseases on mice?’ [Meanwhile] there’s a lot of misinformation, and the public isn’t as well informed about scientific matters as it should be.”
CCS is the leading scientific organization supporting the FDA Modernization Act, a proposed bill which would allow animal testing to continue but also would validate human biology-based methods as approved alternatives to animal testing. Akhtar, who got involved after the legislation was introduced in the House, said most legislators and staff seem “very open” to giving scientists needed options.
“They understand that this bill doesn’t restrict. It only expands options,” she said. “If the United States wants to be a leader in science and technology, we have to do this for innovation.”

Representative Image via Adobe Stock
7 Action Steps Animal Lovers Can Take To Advocate For Animals Used in Labs
If you’re an animal lover upset by the cruel and deadly tests that animals undergo for our continued survival as a species — don’t despair. You can start taking action today to advocate for animals in labs, starting with these seven action steps:
1. Don’t Use Products Tested On Animals When There Are Humane Alternatives
Use your pocketbook to show companies you don’t condone unnecessary cruelty by boycotting soaps, shampoos, cleaners, and other everyday items that have been tested on animals. Both PETA and Leaping Bunny have apps you can download to your phone in order to search for products’ cruelty status while you shop.
2. Sign Our Petitions
If you haven’t already, sign Lady Freethinker’s petition supporting the FDA Modernization Act, which would end FDA requirements established in 1938 to test on animals by validating safer, human-biology-based methods. Also sign our petition demanding that Congress nix a proposed $30 million increase to the National Institutes of Health to breed more monkeys for lab use. We’re also petitioning the European Commission to sign off on a demand from the European Parliament to ban animal testing as soon as possible.
3. Get Educated
There are a number of incredible organizations fighting to stop animals from being used in testing, from cosmetics to medicines, including — but not limited to — the American Anti-Vivisection Society, the National Anti-Vivisection Society, White Coat Waste Project, the European Coalition to End Animal Experiments, People for the Ethical Treatment of Animals, the Coalition for Consumer Information on Cosmetics, Cruelty Free International, and Stop Animal Exploitation Now.
There also are a number of scientific organizations racing to develop safer and more humane alternatives focused on human biology. For those, we recommend checking out the Center for Contemporary Sciences, the Physicians Committee for Responsible Medicine, the Canadian Centre for Alternatives to Animal Methods, and the Center for Alternatives to Animal Testing at Johns Hopkins University.
4. Support Organizations Working to End Animal Testing
Find an organization working to end animal testing, like Lady Freethinker, whose mission you support. Sign up for their action alerts and follow through. Consider donating, if you can, to support their work.
5. Speak Up
Use your social media and other online accounts, your interactions with family and friends and co-workers, and even your car bumper (there are some great stickers out there) to raise awareness about animal testing and the scientists working to develop alternatives.
6. Vote For Compassionate Candidates
Do your research and vote for politicians with proven track records of advocating for animals, including animals used in research.
7. Go Vegan
In addition to saving animals from becoming food, a healthy vegan diet based in whole foods and fresh fruits and veggies has been proven to boost people’s immune systems and decrease the likelihood for some of the conditions — including obesity, hypertension, diabetes, and heart issues — that are associated with severe symptoms of COVID-19 infections. One study reported vegans were 73 percent less likely to be hospitalized or show severe symptoms if infected with the current strains of COVID. The Centers for Disease Control and Prevention also notes that about 75 percent of new diseases start in animals, so by not contributing to demand from filthy and inhumane factory farms, you could also help prevent the next pandemic and the animal testing that likely would be required to come up with new treatments.
IN MEMORIUM. Lady Freethinker honors and thanks all animals who unwillingly suffer and are killed in medical tests and experiments each year. We believe that all beings have an equal right to walk this earth and that all animals have the right to lead lives free from pain, suffering, and exploitation. We will continue to do everything we can to create a more compassionate coexistence and to advocate for safety testing methods that do not involve animal use.








